By: Michael O’Farrell – Investigations Editor
THE HSE has backtracked on its controversial decision not to test all patients being transferred to nursing homes from acute hospitals – more than two-and-a-half months after the sector first asked for the measure.
In the intervening period, more than 1,000 hospital patients were transferred into nursing homes, frequently without tests – even if they were close contacts of Covid-19 victims.
As first revealed by the MoS a month ago, some of those nursing home owners worst hit by the virus blame their outbreaks on these untested hospital transfers.
As recently as this week – with nursing home residents now accounting for more than 62% of all Covid deaths – nursing home sources spoke of their continued struggle to stop untested transfers from hospitals.
One source said: ‘It’s a fight with the hospital to get these people tested. They’re still doing it – this week. This is still going on.’
Last month the MoS highlighted cases in which hospital patients transferred from acute hospitals were subsequently diagnosed Covid-positive – and died – in longterm residential facilities such as Our Lady’s Hospice in Harold’s Cross.
In that instance the hospice had opened unused wards in response to a HSE call for beds as the acute sector was emptied of patients. In another instance the owner of one of the worst-hit nursing homes confirmed that four of the seven hospital transfers his home accepted were found to be positive.
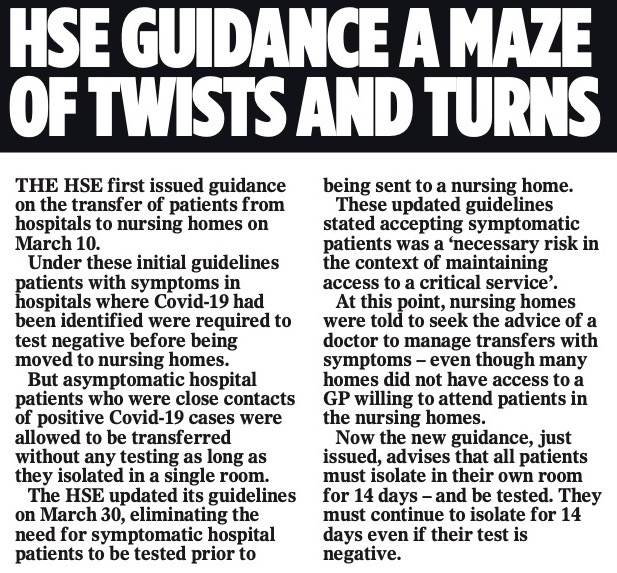
HSE guidance on the testing of transfers from hospitals was first introduced on March 10 and updated on March 30.
But neither set of guidelines called for all transfer patients to be tested, meaning that there was no control of asymptomatic patients coming into nursing homes from hospitals.
Instead, the HSE guidance placed the onus of responsibility on struggling nursing homes who were asked to monitor and isolate transfer patients – often without the availability of an on-site GP.
Now, with Ireland’s nursing home death rate among the worst in the world, the HSE last night confirmed it is finally moving to close that gap.
In a statement to the MoS, a HSE spokesperson confirmed all transfers would now be offered a test as part of revised guidelines to be issued this week.
Last night Nursing Homes Ireland (NHI) chief executive Tadgh Daly welcomed the move but said it had come too late for many.
‘We very much welcome the commitment by the HSE to ensure there is blanket testing of all discharged to nursing homes – no matter how belated it is,’ he said.
‘It’s critical for nursing homes to have full knowledge of everyone coming in because if they do have Covid they are in a position to care for someone in isolation if required.’
Hundreds of pages of records released this week reveal that NHI first asked for all hospital transfers to be tested in early March.
On March 12, two days after the HSE first issued guidance allowing close contacts to be transferred without a test, NHI asked for all transfers to be tested.
‘Nursing homes are, by definition, the facilities in which the most vulnerable citizens in the country are accommodated,’ Mr Daly wrote in a letter to the HSE.
‘Furthermore all the evidence to date highlights that the worst outcomes/prognosis for Covid-19 is in those categories of persons who are most likely to live in nursing homes.
‘It is in this context that we believe it is incumbent on us to do everything possible to reduce the risk of introducing the virus or potential for an outbreak in our nursing homes. We therefore propose it would be prudent to only permit transfer of patients from hospitals where there is evidence of spread of Covid-19 to a nursing home in circumstances where that patient has been confirmed negative for the virus.’
It wasn’t just the nursing homes who mentioned this approach.
A circular, sent by the National Treatment Purchase Fund (NTPF), asked all homes to provide details of capacity ‘to inform national capacity planning for the coming weeks’. ‘All potential residents will be tested and cleared by the hospital of the Covid-19 virus,’ the NPTF’s circular stated.
It appears the NTPF correspondence formed part of the HSE’s deliberate policy of emptying acute hospital patients into long-term residential care to free up hospital capacity.
‘The nursing home will need to have the ability to care for patients coming from an acute hospital setting with a variety of nursing and healthcare needs,’ the circular continues.
Last night the Irish Mail on Sunday asked NTPF chief Liam Sloyne, the HSE and the Department of Health to explain the circular since it is at odds with HSE policy.
There was no response from the HSE or the Department of Health, but a NPTF spokesman did reply: ‘As part of the national response to the Covid-19 outbreak, the NTPF made contact with private nursing homes around the country to help establish capacity within the system.
‘The NTPF made this initial contact as it holds a database of all private nursing homes in the Fair Deal Scheme. The NTPF does not have any responsibility for the transfer of patients from the hospital system to the nursing home system.’
Last night the Irish Bishops’ Conference called for an inquiry into the spread of Covid-19 in nursing homes.
After a critical delay all nursing homes have now been blanket tested – once – though the tests came too late for those worst hit.
Last month the MOS reported how the pleas for blanket testing from the Killbrew and Millbury nursing homes in Meath went unanswered as the virus took double-digit deaths in both locations.
The HSE last night defended its policies saying it is constantly adapting to an evolving and unprecedented crisis.
The service also continues to reject concerns about nursing home outbreaks being caused by hospital transfers, saying simply there is ‘no evidence of this’.
‘Covid-19 is a new disease that health authorities across the world are learning about and adapting to as new evidence and understanding is formed,’ a spokesperson said.
‘The HSE in line with all health authorities continuously reviews emerging evidence and guidance.
‘We are learning as we work through this pandemic and have updated our guidance on several occasions in response to greater understanding of the spread disease. This is changing how we use tests to guide what we advise in relation to nursing homes.’
Our Lady’s Hospice would like to point out that there have been no cases of Covid-19 in its long-term nursing home – Anna Gaynor House – at it’s Harold’s Cross campus. Instead, any Covid cases, in patients transferred from hospital, involved the Hospice’s Community Reablement Unit (CRU)and/or the Rheumatic and Musculoskeletal Disease Unit (RMDU) – both of which are separate from Anna Gaynor House and the Hospice’s palliative care units. During the Covid crisis, the CRU and RMDU are not operating as normal and have been repurposed as step down wards for acute hospital patients.